Advertisement
If you have a new account but are having problems posting or verifying your account, please email us on hello@boards.ie for help. Thanks :)
Hello all! Please ensure that you are posting a new thread or question in the appropriate forum. The Feedback forum is overwhelmed with questions that are having to be moved elsewhere. If you need help to verify your account contact hello@boards.ie
Hi all! We have been experiencing an issue on site where threads have been missing the latest postings. The platform host Vanilla are working on this issue. A workaround that has been used by some is to navigate back from 1 to 10+ pages to re-sync the thread and this will then show the latest posts. Thanks, Mike.
Hi there,
There is an issue with role permissions that is being worked on at the moment.
If you are having trouble with access or permissions on regional forums please post here to get access: https://www.boards.ie/discussion/2058365403/you-do-not-have-permission-for-that#latest
There is an issue with role permissions that is being worked on at the moment.
If you are having trouble with access or permissions on regional forums please post here to get access: https://www.boards.ie/discussion/2058365403/you-do-not-have-permission-for-that#latest
Things for prospective mothers to think about(Contains scientific info on stillbirth)
-
28-04-2011 4:20pm#1Hello all, was reading through another thread in which posters were discussing the importance of natural birth and thought I'd chime in with a few things I think mothers to be should bear in mind, I have moved it from that thread as a regular poster had lost a baby and what comes below would certainly strike a nerve. However, I think it is important enough to bear repeating. I hope the mods don't mind if I move it from the original thread to a new one.
When it comes to pregnancy/childbirth, I think some people place too much emphasis on the experience of childbirth, (i.e. natural vs. C setion, induced or not etc etc.) rather than the outcome. A poor birth experience lasts only a few hours, whereas a poor outcome (dead or disabled child or mother) can have repercussions that last a lifetime.
As a result, obstetricians always place greater emphasis on the outcome. Therefore, when they feel that there is increased risk to the baby by waiting for a natural birth, they will opt to intervene. They do not do this for money, or to keep themselves entertained or anything else. They do it so that mother and child get through the experience unharmed.
It's called labour for a reason, it is difficult and does not always go smoothly. Evolution has given us big brains and upright posture but because of this (big head + narrow female pelvis) human birth is amongst the most difficult in the animal kingdom.
As regards induction, there is very good reason why doctors get pushy once a child is overdue. It is that the incidence of still birth skyrockets past ~40 weeks: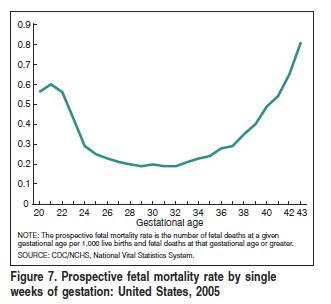
I am currently working on a research project investigating placental function in infants that suffer from neonatal asphyxia. It is possible to tell just from looking at the placenta whether the baby was overdue or not. These placentas are friable, calcified and generally very unhealthy looking. It is this decline in placental function, combined with a growing baby placing increasing demands on the degrading placenta, that causes fetal death in utero.0
Comments
-
My brother in laws sister in law was 40 weeks and 4 days and her baby died inside of her, they wanted her to induced at 40 weeks and 2 days and the hospital said no we wait till your 10 days overdue. ( a uk hospital) If they had of induced her at 40 weeks and 2 days the baby girl would have been born alive. Its very sad. That was only last year.
Ive been very lucky to have all mine before my due date.
* anything can happen at any time, no pregnancy is the same, no baby is the same and no labour is the same, and sometimes doctors/midwifes make the wrong call.
Its weird how a baby born at 32 weeks has a better chance than a baby born at 38 weeks!0 -
grindelwald wrote: »
* anything can happen at any time, no pregnancy is the same.
Its weird how a baby born at 32 weeks has a better chance than a baby born at 38 weeks!
This is very true and something women should keep in mind. Just because your sister/cousin/friend etc had a natural birth doesn't mean you should feel under pressure to have one too.
Do whatever is best for you and your baby.
In answer to the second bit there, a baby at 32 weeks has a better chance of not being stillborn, however, they are more likely to suffer complications of prematurity. This is why people aren't routinely induced at 32 weeks.0 -
Deleted User wrote: »
When it comes to pregnancy/childbirth, I think some people place too much emphasis on the experience of childbirth, (i.e. natural vs. C setion, induced or not etc etc.) rather than the outcome. A poor birth experience lasts only a few hours, whereas a poor outcome (dead or disabled child or mother) can have repercussions that last a lifetime.
A poor birth experience can also last a lifetime and Irish maternity services unfortunately do not accept this. Telling Mothers who have had a difficult experience to just 'get over it' is very disappointing and incredibly difficult to hear even when it's well intentioned. The attitude of 'you should be grateful you have a live baby' does Mothers a huge disservice and I'm sad to see that this sentiment continues in Ireland. Why not help Mothers have safe and fulfilling births?0 -
Deleted User wrote: »
As regards induction, there is very good reason why doctors get pushy once a child is overdue. It is that the incidence of still birth skyrockets past ~40 weeks: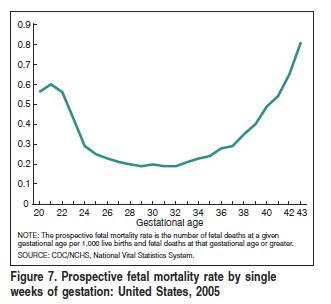
I am currently working on a research project investigating placental function in infants that suffer from neonatal asphyxia. It is possible to tell just from looking at the placenta whether the baby was overdue or not. These placentas are friable, calcified and generally very unhealthy looking. It is this decline in placental function, combined with a growing baby placing increasing demands on the degrading placenta, that causes fetal death in utero.
Does this only occur past 40 weeks?
I've also seen placentas from 'overdue' Mums which have been perfectly healthy and I've seen placentas before EDD with massive calcification due to other factors (smoking). Personally I would not look to US studies on neonatal mortality given the huge inequalities in antenatal care and preterm birth rates. There are some Swedish post term studies that I'm sure you're aware of that would contradict your theory.0 -
-
Advertisement
-
Deleted User wrote: »Because very occasionaly, and unfortunately, the two are mutually exclusive.
If it is very occasionally, then why should it be treated as if it is the norm?
Childbirth is a normal physiological event. We've all heard the phrase that childbirth can only be declared normal in retrospect, but for the majority of women, being allowed to go into labour spontaneously and being allowed to labour for as long as is normal for her will lead to the birth of a healthy baby. 40 weeks is the average gestation period and should not be taken as normal for all women. If a woman has a normal gestation period of 38 weeks, then at 40 weeks she is already significantly overdue and is of course at greater risk of placental deterioration and stillbirth. However for those women who would have a normal gestation period of 42 weeks, at 40 weeks their baby and placenta will be doing just fine. The problem with current procedure is that all women seem to be expected to conform to a norm that is not necessarily normal for them.
It is terrifying when you are expecting a baby and you are deemed to be overdue and you are told that you are putting your baby's life at risk if you don't agree to various interventions. I myself experienced this. There were no indications that my child was in anyway compromised but I was constantly told by doctors who had barely examined me that I was endangering him. In the event, I was induced at 40 + 10. After an intense and short labour I gave birth to a fine healthy baby boy and a perfect placenta. He nor it showed no signs of postmaturity or trauma of any kind. I, on the other hand, had torn very badly because of the speed of the induced labour - on the basis of my Bishop's score I was far from an ideal candidate for induction (no softening of cervix, no effacement, baby still very high) and I was lucky to have avoided a c-section.
I was also very lucky in that I had a team of midwives who knew I wanted as natural a birth as possible and supported me through it, and who seemed to keep the doctors at bay. Maybe that meant there were greater risks to my child and myself, but in any case, the trip down the birth canal is one of the riskiest journeys we take in life.
If I had to choose, of course I would rather have tearing and a healthy baby than no baby, but what if we had been allowed to progress normally? Why is admission and monitoring not an alternative to immediate intervention? It may be overly cynical on my part, but I have a strong suspicion that a lack of beds, staff and resources have more to do with the active management of labour than evidence-based research has.
In utero death is not only caused by placental degradation - congenital malformation is a much more common cause. Some stillbirths are due to infection, or accidents, or (very few) due to the process of birth itself. The majority are simply unexplained - life and death is a still a mystery after all.
Like some of the others, I feel your defence of current obstetrical practice complete with all of it's interventions is misguided and unnecessary. every pregnant woman in Ireland will run the gauntlet of 'birth management', arbitrary deadlines and routine interventions, unless she is lucky enough to have a hands-off care provider. Yes, women need to be aware of the risks, but they also need to be allowed to choose the level of risk they are comfortable with. Litigation-wary doctors are maybe not best placed to decide what is best for a normally progressing but overdue mother-to-be.0 -
I disagree. In research on traumatic births it's not necessarily about the medical care/interventions that took place but how the Mothers were treated. Kindness costs nothing and a little sensitivity goes a long way.0
-
Cat Melodeon wrote: »It is terrifying when you are expecting a baby and you are deemed to be overdue and you are told that you are putting your baby's life at risk if you don't agree to various interventions. I myself experienced this. There were no indications that my child was in anyway compromised but I was constantly told by doctors who had barely examined me that I was endangering him. In the event, I was induced at 40 + 10. After an intense and short labour I gave birth to a fine healthy baby boy and a perfect placenta. He nor it showed no signs of postmaturity or trauma of any kind. I, on the other hand, had torn very badly because of the speed of the induced labour - on the basis of my Bishop's score I was far from an ideal candidate for induction (no softening of cervix, no effacement, baby still very high) and I was lucky to have avoided a c-section.
If I had to choose, of course I would rather have tearing and a healthy baby than no baby, but what if we had been allowed to progress normally?
Why is admission and monitoring not an alternative to immediate intervention?
.
Just to say i tore very bad with my second guy a 3rd degree tear and he wasnt induced he was 5 weeks prem (the 3rd guy redid all the damage and did a little more) . inducement doesn't necessarily lead to tears and natural labour can result in a tear. Some natural labours are worse than induced labours, depends on the person.
Admission and monitoring would have to be 24/7 that's a lot of monitoring for a maternity hospital. The baby heart beat could stop at any time day or night it would mean a rush to get the c-section done and maybe resuscitation needed and pediatricians there. if the mother has a full stomach then there would be a risk during anesthetic. To me its still safer to induce at 41 weeks.
Im lucky ive had mine all early but i was always prepared to die for my baby's if needs be, if that meant emergency c-section or inducement Or anything else as long as baby was ok i didn't care about myself.0 -
Does this only occur past 40 weeks?
I've also seen placentas from 'overdue' Mums which have been perfectly healthy and I've seen placentas before EDD with massive calcification due to other factors (smoking). Personally I would not look to US studies on neonatal mortality given the huge inequalities in antenatal care and preterm birth rates. There are some Swedish post term studies that I'm sure you're aware of that would contradict your theory.
My placenta was perfect, as was our baby, nothing "post dates" about either of them.
Three full scans in the space of 5 days, over a week of extreme pressure to agree to an induction that even the consultants agreed was not medically indicated (scan results were 8/8 on all three, chord was functioning perfectly, plenty of fluid, CTG were fine etc.) and the consequential result that putting me in "flight or fight" mode periodically (resulting in over a week of stop-start labour) had on my ability to maintain labour, seem to me to be the most likely causes of the death of our baby, and this opinion has been shared by healthcare professionals who are aware of my history and the events of the past few weeks.
Every woman is different, as is every pregnancy, and each should be assessed as individual and unique, not on the basis of case studies, averages or other statistics. I'm not a statistic, and my baby shouldn't have ended up as one.
Maternity care in this country needs to be reviewed, I find it ironic that I had the best (hospital based) birth experience of anyone I know and that it was only because my baby was dead. It seems that the best way to get compassionate considerate hospital maternity care is to lose your child :eek::P0 -
Cat Melodeon wrote: »If it is very occasionally, then why should it be treated as if it is the norm?
Car crashes happen only very occasionally, but we still wear seatbelts.
As for congenital malformations, they tend to cause early miscarriage, not stillbirth. You are right that many cases of death in utero are never explained, but there is a proven correlation between being overdue and stillbirth.
Admission and monitoring would be fairly pointless. Even if it were noticed the minute the fetal heart stopped beating it would be almost impossible to get the baby out in time to resuscitate it.0 -
Advertisement
-
Deleted User wrote: »
Admission and monitoring would be fairly pointless. Even if it were noticed the minute the fetal heart stopped beating it would be almost impossible to get the baby out in time to resuscitate it.
Not necessarily. The placenta doesn't one minute stop being able to support the growing infant. There is a gradual decline in placental function. Signs of this could be picked up with CTG monitoring - low base rate, lack of accellerations and movements, poor variability. If a woman has gone overdue and understands the risks, why shouldn't she be offered this little bit of extra monitoring? Admission wouldn't always be necessary if the woman can attend her local maternity hosptal daily or twice daily. Most women probably would opt for induction, but those who really want to labour spontaneously and have as natural a birth as possible should be supported within reason to do so!0 -
crazy cat lady wrote: »Not necessarily. The placenta doesn't one minute stop being able to support the growing infant. There is a gradual decline in placental function. Signs of this could be picked up with CTG monitoring - low base rate, lack of accellerations and movements, poor variability. If a woman has gone overdue and understands the risks, why shouldn't she be offered this little bit of extra monitoring? Admission wouldn't always be necessary if the woman can attend her local maternity hosptal daily or twice daily. Most women probably would opt for induction, but those who really want to labour spontaneously and have as natural a birth as possible should be supported within reason to do so!
If CTG abnormalities are picked up what does it lead to- an induction or c section. Monitoring on an oupatient basis is useless really, it reveals only the fetal health at that moment in time, and has no predictive value for future survival.
Even aside from the stillbirth risks there are plenty of reasons to avoid going significantly overdue (>42 wks):
Problems during labour due to larger fetus (25% >4000g)
Fetal skull more ossified and less easily moulded
Passage of meconium (25-42%)
Neonatal death 3x more likely
Neonatal seizures 10x more likely
All of these additional risks, for what?0 -
Over 42 weeks, fine, there is plenty of evidence for that, but many women start to feel pressurised by doctors long before that when there is no medical indication of a problem.Deleted User wrote: »Even aside from the stillbirth risks there are plenty of reasons to avoid going significantly overdue (>42 wks):Deleted User wrote: »Car crashes happen only very occasionally, but we still wear seatbelts.
Ridiculous metaphor. You cannot compare unnecessary interventions that quite often lead to major abdominal surgery and which impact on the development of the child to the wearing of a seatbelt.
A better analogy would be the example of children in the 30s who had all of their perfectly healthy teeth extracted and replaced with dentures in order to avoid tooth decay, or entire families who would have their tonsils and adenoids removed in case of infections (where there was no history of such infections.
Women need to be dealt with on an individual basis and measured against their own medical history. Where interventions are necessary, they should be performed, but only when all other options have been explored.
An emergency is an emergency, none of us would wish that on anyone, and that is where intervention has its place. Advocating for the medicalisation of birth over more natural, normal birth when there is a significant and growing body of evidence-based research to suggest that this is not best practice seems perverse.0 -
My placenta was perfect, as was our baby, nothing "post dates" about either of them.
Three full scans in the space of 5 days, over a week of extreme pressure to agree to an induction that even the consultants agreed was not medically indicated (scan results were 8/8 on all three, chord was functioning perfectly, plenty of fluid, CTG were fine etc.)
Same as my brother in law sister inlaw, one day she was fine and healthy all going well, the next she was dead, seems no reason for it the heart stopped beating but it did.
That makes me wonder if an unborn baby could suffer with SIDS, a woman i know whos baby was 1 week old died from SIDS if that child had still been inside her would it have died? who knows, still very tragic.0 -
Cat Melodeon wrote: »
Ridiculous metaphor. You cannot compare unnecessary interventions that quite often lead to major abdominal surgery and which impact on the development of the child to the wearing of a seatbelt.
A better analogy would be the example of children in the 30s who had all of their perfectly healthy teeth extracted and replaced with dentures in order to avoid tooth decay, or entire families who would have their tonsils and adenoids removed in case of infections (where there was no history of such infections.
.
Better analogy would be ovarian cancer its more of a life death situation, you cant compare the risk of a stillbirth to risk of tonsillitis or risk of tooth decay!
I think the seat belt analgoy rings true, some will crash and die and others will crash and survive ( of those that survive some will be fine fit n healthy and some will have long term complications others short term) others wont crash at all. I think its a perfect analogy.0 -
grindelwald wrote: »Better analogy would be ovarian cancer its more of a life death situation, you cant compare the risk of a stillbirth to risk of tonsillitis or risk of tooth decay!
I think the seat belt analgoy rings true, some will crash and die and others will crash and survive ( of those that survive some will be fine fit n healthy and some will have long term complications others short term) others wont crash at all. I think its a perfect analogy.
I'm not comparing tooth decay to stillbirth, I'm making the point that arbitrarily conducting interventions when they are not medially indicated simply because of an artificially imposed time limit should not be standard practice, just as in the past procedures were carried out routinely which seem barbaric now and which would never be considered by doctors today.
We all know that driving a car is one of the riskiest things we do each day. Wearing a seat belt is the sensible thing to do and it does not cause any harm to the wearer. Having a baby carries less risk (in terms of outcomes) than driving. Treating interventions such as induction or c-section as being a commonplace safety measure equivalent to wearing a seatbelt seems to denigrate the rights of the woman to physical safety and basic dignity. Interventions can be violent and scarring. They should not be commonplace.0 -
I will be very doubtful of all this theory until they devise a way of being more precise about due dates and gestation periods.0
-
I trust the evidence.
The evidence shows us that stillbirth increases from 42 complete weeks. Not 40 weeks. Many hospitals have brought their post date policy in line with this evidence.
ESRI states, "In 2008 approximately 1 in every 200 births were stillborn and 1 in every 470 live births died in the first week of life. ESRI States: Despite improvements in reducing perinatal mortality in recent decades, the perinatal period continues to be a time of relatively high risk. "
The same ESRI report indicates a concerning increase in medical intervention and Caesarean section rate of nearly 27%
The evidence also shows us that routine medical intervention and caesaren section contributes to perinatal and maternal mortality and morbidity.
* Only 43.5% of First time mothers will have a spontaneous birth. (WHO recommends 85%). Down from 50.7% in 1999.
* 7.2% of First Time Mothers will have a forceps delivery. This is down from 8.1% in 1999 BUT UP from 5.1% in 2004
* 21.4% of First Time Mothers will have a vacuum extraction. This is Up from 17.0% in 1999.
* 27.3% of First Time Mothers will have a Caesarean Section. This is UP from 23.2% in 1999.
Birth experience matters. The second highest contributor to maternal death is suicide following the first post natal year. This is widely believed to be down to an increase in PTSD, PND, birth related trauma and lack of services to evaluate a mother's mental health following birth.
Sqiggler, I am so very sorry for your loss.0 -
^ I hope they bring more attention to post natal care. In my experience you get lots of care and attention for pre-natal, and then after the baby is born there is zero care, except for some iron tablets, which imo is entirely inadequate for the shell shock of new motherhood. Sometimes I dont know how I made it through the first year.0
-
* Only 43.5% of First time mothers will have a spontaneous birth. (WHO recommends 85%). Down from 50.7% in 1999.
* 7.2% of First Time Mothers will have a forceps delivery. This is down from 8.1% in 1999 BUT UP from 5.1% in 2004
* 21.4% of First Time Mothers will have a vacuum extraction. This is Up from 17.0% in 1999.
* 27.3% of First Time Mothers will have a Caesarean Section. This is UP from 23.2% in 1999.
Birth experience matters. The second highest contributor to maternal death is suicide following the first post natal year. This is widely believed to be down to an increase in PTSD, PND, birth related trauma and lack of services to evaluate a mother's mental health following birth.
Sqiggler, I am so very sorry for your loss.
It's true intervention rates have increased significantly, but in direct correlation, perinatal mortality has dropped correspondingly.
"Among 176,620 non-anomalous births the corrected perinatal mortality fell from 10.6 in 1984 to 7.4 /1000 in 200724.8% (p<0.001)."
(p<0.001). The caesarean section rate increased from 4.2 % to 18.9% and the induction rate increased from 10.8% to
So despite the fierce oppostion to any form of medical intervention that seems to prevail on here, there is no denying that increasing amounts of intervention has saved the lives of countless babies.0 -
Advertisement
-
Deleted User wrote: »So despite the fierce oppostion to any form of medical intervention that seems to prevail on here, there is no denying that increasing amounts of intervention has saved the lives of countless babies.
James I think you've misunderstood the sentiments expressed here - while I can only speak for myself I am not opposed to medical intervention - when it is necessary.....it's the routine over use of intervention that is not supported by evidence (ie routine breaking of waters, routine induction episiotomies etc that I have difficulty with).
New research published in the April issue of The Journal of Maternal-Fetal and Neonatal Medicine suggests that intervention is not linked tohealthier babies.
http://www.sciencedaily.com/releases/2011/04/110413101916.htm0 -
James - you missed the key word in my post, "routine"
I have no problem whatsoever with medically indicated intervention or caesarean section. I can even understand certain arguments with regards to informed choice and maternally requested intervention/caesarean.
However, we know routine intervention does not save babies.
In fact, research shows that routine intervention is associated with significant increased risks to mother and baby.
We also know that new research has shown that levels of high intervention do not improve outcomes for infants.
http://www.sciencedaily.com/releases/2011/04/110413101916.htm0 -
apologies for the repost of link!0
-
That's a U.S. study, not sure how relevant it is to obstetric practice in Ireland, given that their C section rate was 32% in 2007 as opposed to 18.9% here. I suspect a significant proportion of C sections there (as here) are elective.
These climbing C section rates are a worrying trend, as C sections have an increased risk of maternal complications.
This, however, is a completley different issue to non elective or emergency C section, which is only performed when there is a definite need for it.
Induction is a seperate issue again, and the risks of going post dates has been shown over and over again in countless large studies from around the world.
While induced labour is more likely to result in C section there is a confounding factor here:
A higher proportion of induced babies will be post dates, and thus on average bigger than their non induced counterparts. Also, being post-mature their skulls will be more ossified, less easily moulded, and more prone to obstructed labour.0 -
Cat Melodeon wrote: »I'm not comparing tooth decay to stillbirth, I'm making the point that arbitrarily conducting interventions when they are not medially indicated simply because of an artificially imposed time limit should not be standard practice, just as in the past procedures were carried out routinely which seem barbaric now and which would never be considered by doctors today.
We all know that driving a car is one of the riskiest things we do each day. Wearing a seat belt is the sensible thing to do and it does not cause any harm to the wearer. Having a baby carries less risk (in terms of outcomes) than driving. Treating interventions such as induction or c-section as being a commonplace safety measure equivalent to wearing a seatbelt seems to denigrate the rights of the woman to physical safety and basic dignity. Interventions can be violent and scarring. They should not be commonplace.
If that time limit were not in place they would be many more dead babies and many more grieving moms, they are not doing it for the fun of it they are concerned for both mother and babies safety.
A the end of the day its the mothers choice, no one can force her to have an intervention.
On your second point what about the babies right to life? you seem to be thinking of only the carrier and not the life inside!0 -
I would understand medical intervention if the dates were definitive and there was any indication that the baby or mother may be at risk. However, as in my 2 pregs, dates can very easily & commonly be miscalculated.
My first preg was 41 weeks, leading the docs to start talking induction, but when my daughter was born the midwife commented on the amount of white vernix she still had (apparently it's mainly gone at term, and certainly at 41 weeks). This would indicate that the preg may not have been 41 weeks afterall, and if I'd been induced...:(
The due dates of my second preg differed by 10 days...the EDD by missed-period calculation was 10 days before the EDD determined by the scan. So when I was "over" by 13 days by dates, I was only 3 days over by scan. They wanted to induce me then too, but it wound up not being necessary.
James, I think everyone here will easily support any effort to deliver a healthy baby safely. But at what point can you definitively define "overdue?" If, in my cases, the preg isn't really overdue, there's a risk to mom & baby by delivering under unspontaneous conditions.0 -
James, I think everyone here will easily support any effort to deliver a healthy baby safely. But at what point can you definitively define "overdue?" If, in my cases, the preg isn't really overdue, there's a risk to mom & baby by delivering under unspontaneous conditions.
Dating scan is much more accurate than LMP based calculation. The risks assocciated with being induced a week or so early are considerably less than those associated with going a week or more over.
By the way, it's standard practice to book women in for an induction at term + 10 days. Just because they book you in does not mean they think you will need to be induced. It's just so that the arrangements are in place if you do go that late. Even after being booked in, the majority of women go into labour spontaneously before the date the induction is booked for.0 -
Deleted User wrote: »That's a U.S. study, not sure how relevant it is to obstetric practice in Ireland, given that their C section rate was 32% in 2007 as opposed to 18.9% here. I suspect a significant proportion of C sections there (as here) are elective.
These climbing C section rates are a worrying trend, as C sections have an increased risk of maternal complications.
This, however, is a completley different issue to non elective or emergency C section, which is only performed when there is a definite need for it.
Induction is a seperate issue again, and the risks of going post dates has been shown over and over again in countless large studies from around the world.
While induced labour is more likely to result in C section there is a confounding factor here:
A higher proportion of induced babies will be post dates, and thus on average bigger than their non induced counterparts. Also, being post-mature their skulls will be more ossified, less easily moulded, and more prone to obstructed labour.
James, Ireland's Caesarean section rate is nearly 27% (26.7%). Not 18%. A large proportion of these Caesarean Sections are indeed elective due to failure to provide breech clinics and a lack of VBAC options (some units rank in at only a 4.5% vbac rate as compared to guidelines of 70%) but a significant proportion come from induction of labour and effects of oxytocin. The fact is, our maternity services are becoming more closely in line with places like the US. Highly medicalised, highly obstetric, majority of women solely have access to consultant led care IE. birth becomes a medical event with a surgeon.
That research is not for electives alone.
Using statistical models, Glantz assessed the relationship between rates of induction and cesarean delivery and rates of the three neonatal outcomes. He found intervention rates had no consistent effect on newborns: Whether a hospital did a lot or very few interventions, there was no association with how sick or healthy the infants were.
Even after a second round of analysis that accounted for differences among pregnant women that could potentially impact the results, the finding was the same -- hospitals with high intervention rates had newborn outcomes indistinguishable from hospitals with low rates.
According to Glantz, "If higher intervention rates were preventing negative outcomes that otherwise would have occurred, and lower intervention rates led to negative outcomes that potentially could have been avoided, the data would have revealed these relationships, but there were no such trends."
On induction:
There is high quality internationally recognised evidence which shows us that stillbirth increases from 42 complete weeks. Irish maternity units (well some....) have come in line with this evidence and newer induction policies reflect this; ie induction at term+14.
There is a new phenomenon occurring in units who don't consult the evidence. Premature induction. Babies induced too soon and suffer adverse affects as a result. Ask any midwife, due to an over-reliance of technology babies are being born covered in vernix and requiring nicu following inappropriate uses of induction0 -
Deleted User wrote: »Dating scan is much more accurate than LMP based calculation. The risks assocciated with being induced a week or so early are considerably less than those associated with going a week or more over.
Women Ireland do not have access to dating scans. Booking in appointments in Ireland range from 12 weeks to 20+wks in some units.
Inaccuracies for fetals scanning is widely reported. The later in a pregnancy a woman is assessed, the higher the rate of inaccuracies. The rate with which a scan can vary is +/- 1 to 3lbs depending on when in pregnancy the scan takes place. With estimated gestation for EDD by scans, inaccuracies increase after the first trimester and become dependent on genetic/conditional factors0 -
Advertisement
-
James, Ireland's Caesarean section rate is nearly 27% (26.7%). Not 18%.
Ok thanks, didn't know that, where did you get that figure? (Not doubting its accuracy, just curious.)
I agree it would be terrible to see obstetric practice take the same route it has in the U.S. (section first, ask questions later), but at the same time the evidence as regards post maturity is too strong to ignore, and while adopting policies aimed first and foremost at preventing postmaturity related stillbirths will result in some women having less than perfect experiences, it also saves lives.0 -
Women Ireland do not have access to dating scans. Booking in appointments in Ireland range from 12 weeks to 20+wks in some units.
Inaccuracies for fetals scanning is widely reported. The later in a pregnancy a woman is assessed, the higher the rate of inaccuracies. The rate with which a scan can vary is +/- 1 to 3lbs depending on when in pregnancy the scan takes place. With estimated gestation for EDD by scans, inaccuracies increase after the first trimester and become dependent on genetic/conditional factors
Early scans are very accurate. It is a pity that some women have to wait so long for them that they are done when they are no longer as accurate.0 -
Deleted User wrote: »Ok thanks, didn't know that, where did you get that figure? (Not doubting its accuracy, just curious.)
I agree it would be terrible to see obstetric practice take the same route it has in the U.S. (section first, ask questions later), but at the same time the evidence as regards post maturity is too strong to ignore, and while adopting policies aimed first and foremost at preventing postmaturity related stillbirths will result in some women having less than perfect experiences, it also saves lives.
2008 Perinatal Stats - ESRI
"The trend in delivery by caesarean section has increased from 20.4 per cent in 1999 to 26.7 per cent for total live births in 2008, (for total maternities 20.0 per cent in 1999 and 25.9 per cent in 2008)."0 -
apologies, misread post, (deleted)0
-
I found this thread very interesting.
I kind of had the opposite to what most mothers do, I felt i should have been talked to more about being induced.
I was overdue by 2 weeks. I went into labour the day before I was due to be induced (which would have been 15 days over).
At 39 weeks they discussed induction if i was to go over 40 and then I remember having two check ups in those 2 weeks that i was overdue, one including a scan to check the fluid, and they kept saying vague statements like 'if you go over by too long will have to induce' they never difinitively said we'll induce you after X amount of days, which i thought was weird. eventually they set the date when i was 13 days over.
i was actually relieved that they were showing signs of caring!
I had not 'dropped' even when labour started, baby was still very high and it took 29 hours of painful contractions to drop first and then the actual labour. so maybe that had something to do with not being induced?
After the birth the midwife commented on the placenta being 'ragged' but never went into detail. would you say theres some connection there?
i think alot of mothers set their heart on the all natural birth,and i think thats all well and good but if a doctor feels you need some sort of assistance then they should accept that. obviously there are exceptions to that, and a woman knows her body and her baby, so if she genuinely feels its not right then she should speak up, but im talking about mothers who outright from the start are determined to do it all their way regardless of what they're told is best.
i think it should be stressed that birth plans are more birth 'ideals'. that they are what you should consider the best case scenario but not necessarily what should be expected.0 -
My second son had a ragged placenta, he was born 5 weeks early, it means the placenta did not come away cleanly and you might need a d&c. my womb wasnt contracting down as normal and the PHN came evry day to check on me it was only on the 6th day that she was happy that no bit of placenta was left behind.0
-
Advertisement
-
grindelwald wrote: »My second son had a ragged placenta, he was born 5 weeks early, it means the placenta did not come away cleanly and you might need a d&c. my womb wasnt contracting down as normal and the PHN came evry day to check on me it was only on the 6th day that she was happy that no bit of placenta was left behind.
thanks for that.
this is what i thought too. that bits may have come apart from it.
thing is, i was never checked or even told what it meant. and i was a sixteen year old child at the time so there wasnt a chance they assumed i knew. it was just said to me in passing and never mentioned again!0 -
Deleted User wrote: »the evidence as regards post maturity is too strong to ignore
Could you cite your information?
WHO define "prolonged pregnancy" as continuing after 42 weeks. ie term+14
Cochrane says:
A policy of labour induction after 41 completed weeks or later compared to awaiting spontaneous labour either indefinitely or at least one week is associated with fewer perinatal deaths. However, the absolute risk is extremely small. Women should be appropriately counselled on both the relative and absolute risks
http://www2.cochrane.org/reviews/en/ab004945.html
And when you look at the absolute risk of perinatal death its 0.03% for the induction group and 0.33% for the non-induction group. Less than 0.5% risk for inducing or not. Hardly too strong to ignore.....which is probably why best practice says non-medically indicated induction should be offered at term+140 -
James, I think everyone here will easily support any effort to deliver a healthy baby safely. But at what point can you definitively define "overdue?" If, in my cases, the preg isn't really overdue, there's a risk to mom & baby by delivering under unspontaneous conditions.
Is it better to be safe than sorry!
One minute baby is fine, next the baby is dead. Who is to tell when baby's heart is going to stop, it could easily stop the minute you leave the doctors from the check up.
If science could predict when baby's heart is going to give in (or placenta stops working) then there would be no need for such interventions until medically necessary, again is it not better to be safe than sorry, to take action before an emergency arises.0 -
Could you cite your information?
WHO define "prolonged pregnancy" as continuing after 42 weeks. ie term+14
Cochrane says:
A policy of labour induction after 41 completed weeks or later compared to awaiting spontaneous labour either indefinitely or at least one week is associated with fewer perinatal deaths. However, the absolute risk is extremely small. Women should be appropriately counselled on both the relative and absolute risks
http://www2.cochrane.org/reviews/en/ab004945.html
And when you look at the absolute risk of perinatal death its 0.03% for the induction group and 0.33% for the non-induction group. Less than 0.5% risk for inducing or not. Hardly too strong to ignore.....which is probably why best practice says non-medically indicated induction should be offered at term+14
Now we're getting into the difference between relative and absolute risk. Yes the absolute risk is small but going from the figures above the relative risk is 11x greater.0 -
grindelwald wrote: »Is it better to be safe than sorry!
One minute baby is fine, next the baby is dead. Who is to tell when baby's heart is going to stop, it could easily stop the minute you leave the doctors from the check up.
If science could predict when baby's heart is going to give in (or placenta stops working) then there would be no need for such interventions until medically necessary, again is it not better to be safe than sorry, to take action before an emergency arises.
this, i think, is my stance on the issue.
i think you're damned if you do, you're damned if you dont.
sometimes the decision is the wrong decision, which is obviously heartbreaking, but if they werent to take action and the outcome was the same they'd still be to blame.
and it'd be my understanding that if they were to induce they'd have more medical 'scope'(???) to help if anything went wrong than if baby was left in the womb and they couldnt give it medical attention. if that makes sense.0 -
Advertisement
-
Could you cite your information?
WHO define "prolonged pregnancy" as continuing after 42 weeks. ie term+14
Cochrane says:
A policy of labour induction after 41 completed weeks or later compared to awaiting spontaneous labour either indefinitely or at least one week is associated with fewer perinatal deaths. However, the absolute risk is extremely small. Women should be appropriately counselled on both the relative and absolute risks
http://www2.cochrane.org/reviews/en/ab004945.html
And when you look at the absolute risk of perinatal death its 0.03% for the induction group and 0.33% for the non-induction group. Less than 0.5% risk for inducing or not. Hardly too strong to ignore.....which is probably why best practice says non-medically indicated induction should be offered at term+14
14 April 2011 - Some 2.6 million stillbirths occurred worldwide in 2009, according to the first comprehensive set of estimates published in a special series of The Lancet. Every day more than 7200 babies are stillborn — a death just when parents expect to welcome a new life — and 98% of them occur in low- and middle-income countries. Well-known interventions for improving maternal and newborn health would reduce the number of stillbirths too. Well-known interventions for women and babies would save stillbirths too
The Series shows that the way to address the problem of stillbirth is to strengthen existing maternal, newborn, and child health programmes by focusing on key interventions, which also have benefits for mothers and newborns.
According to an analysis to which WHO contributed in The Lancet Stillbirth Series, as many as 1.1 million stillbirths could be averted with universal coverage of the following interventions:
Intervention Stillbirths averted
Identification and induction for mothers with >41 weeks gestation 52000
http://www.who.int/reproductivehealth/topics/maternal_perinatal/stillbirth/Press_release_stillbirths_2011/en/index.html0 -
I was two weeks overdue according to the experts, but looking back I think they got it way way way wrong and as a result I had every intervention imaginable and a baby born too early, my guess is as much as a month too early.0
-
-
I found this thread very interesting.
I kind of had the opposite to what most mothers do, I felt i should have been talked to more about being induced.
I was overdue by 2 weeks. I went into labour the day before I was due to be induced (which would have been 15 days over).
At 39 weeks they discussed induction if i was to go over 40 and then I remember having two check ups in those 2 weeks that i was overdue, one including a scan to check the fluid, and they kept saying vague statements like 'if you go over by too long will have to induce' they never difinitively said we'll induce you after X amount of days, which i thought was weird. eventually they set the date when i was 13 days over.
i was actually relieved that they were showing signs of caring!
I had not 'dropped' even when labour started, baby was still very high and it took 29 hours of painful contractions to drop first and then the actual labour. so maybe that had something to do with not being induced?
After the birth the midwife commented on the placenta being 'ragged' but never went into detail. would you say theres some connection there?
i think alot of mothers set their heart on the all natural birth,and i think thats all well and good but if a doctor feels you need some sort of assistance then they should accept that. obviously there are exceptions to that, and a woman knows her body and her baby, so if she genuinely feels its not right then she should speak up, but im talking about mothers who outright from the start are determined to do it all their way regardless of what they're told is best.
i think it should be stressed that birth plans are more birth 'ideals'. that they are what you should consider the best case scenario but not necessarily what should be expected.
Ragged placentas are also caused by 'mismanagement' of the 3rd stage of labour.....cord traction and the placenta being pulled out before it has completely separated (which can sometimes result in a serious bleed too as the uterus can't clamp down properly).0 -
metrovelvet wrote: »I was two weeks overdue according to the experts, but looking back I think they got it way way way wrong and as a result I had every intervention imaginable and a baby born too early, my guess is as much as a month too early.
How far along were you when you did your pregnancy test? missed 1, 2, or 3 or more periods?
That would give you a good idea when you were likely to have conceived and when baby would be due giving that average gestation for a human is 40 weeks. I know when i ovulate as I'm in that much pain i cant walk so all my dates have been spot on, suppose im one of the lucky ones..... even my guy who was 5 weeks early was perfect (plastered in vernix) and was let home at 26 hours old.
Most people take the test 1 week after missed period.0 -
-
I agree with a lot of the sentiment in the opening post. I would place birth outcome over experience any day. I had a pretty eventful birth, but I really didn't care about my experience, the only thing I cared about was a healthy baby. Of course, I'm not saying mothers who want a positive experience don't want the same thing, but for me, I believe a negative or harsh birth experience I can get over. The loss of a baby, I very much doubt I could recover from.
Whilst of course there are parts of childbirth that need to be address in this country, and there does seem to be a lot of reform with early transfer home schemes etc, but I think the area that needs to be addressed is miscarriage. When I had a miscarriage in November I went to Holles Street and was left sitting in a corridor like a leper for an hour and a half segregated from the other mums. It was like they were the 'A' students and i was the failure. After two scans I was told there was still bits of tissue there but they patted me on the head sent me packing with some antibiotics and told me to take a pregnancy test in a couple of weeks and it all should be gone by then. Like it was nothing. A little compassion would have been nice.0 -
On the topic of scans, if the equipment is not sensitive enough or if the staff is not well-trained enough to determine whether a fetus is alive or dead, as recent reports have shown is the case in at least one Irish hospital, then I do not have very much confidence in them being sensitive/skilled enough to determine fetal age accurately either.grindelwald wrote: »If that time limit were not in place they would be many more dead babies and many more grieving moms, they are not doing it for the fun of it they are concerned for both mother and babies safety.
A the end of the day its the mothers choice, no one can force her to have an intervention.
On your second point what about the babies right to life? you seem to be thinking of only the carrier and not the life inside!
Grindelwald, I feel you are deliberately misconstruing what I am saying. I am not advocating for no interventions, only for more considered application of them and for women to be treated on a case by case basis, not for them to be treated as a homogenous group.
No woman would deliberately put her child's life at risk, but why should she be encouraged/coerced to undergo interventions in situations where there is no clear evidence that it is necessary? Yes, err on the side of caution, but not to the extent that unnatural birth becomes the norm, as is fast becoming the case for first-time mothers.
As to the second point, I'm not going to get into a right to life argument on here as that is a separate and extremely emotive issue, but for the record, I absolutely believe that the life of the mother has priority over that of the child. I do not believe that the mother has a right to refuse necessary interventions when that clearly endangers the baby's life however, I hope that distinction is clear.0 -
...and while they may not be doing them for the fun of it...there are financial motivations..
1.fear of litigation
2. C sections in the US are 25K
cat mel is right. Intervention is becoming more and more the norm. If my brother and I were born today, we would have both ended up as sections.0 -
grindelwald wrote: »wonder is they are pre planned, medically necessary or emergency sections?
would seem that this would be a hospital for high risk pregnancies where intervention is needed.
Kilkenny - a small regional hospital. In Lagan Valley unit in the North Dr Niamh McCabe was able to reduce the c-section rate from 22% to 14% with no increase in neonatal mortality.0 -
Advertisement
Advertisement